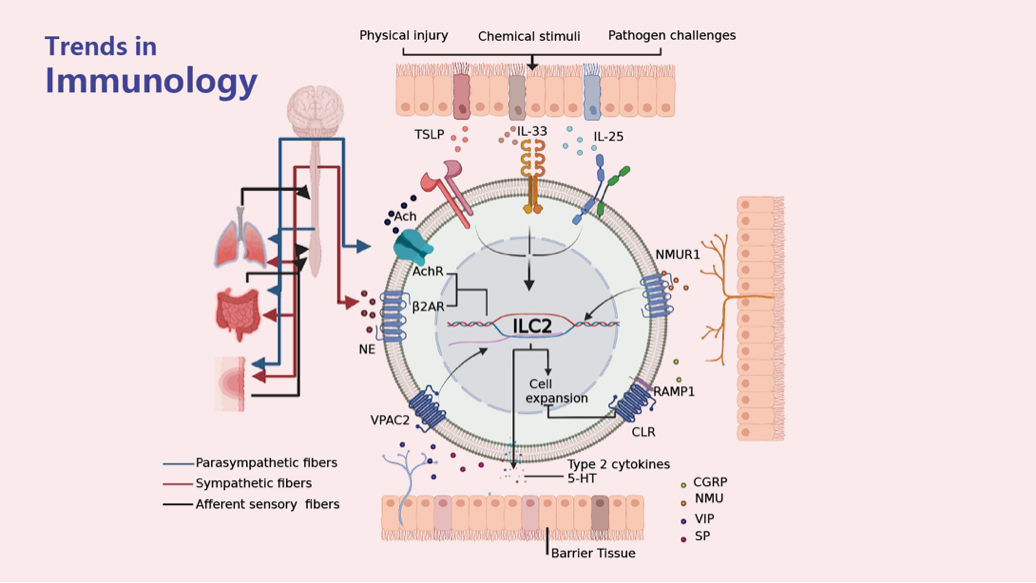
To maintain tissue homeostasis, group 2 innate lymphoid cells (ILC2s) exert pleiotropic functions and have effects on pathogen clearance, tissue injury, and disease development in humans and mice. Epithelial cytokines trigger ILC2s, whereas neuronal signals have dichotomous effects on ILC2-centered networks in humans and mice.
But further studies are required to understand better how ILC2s contribute to maintaining tissue homeostasis in the skin, lungs, and gut. Conventional concepts define inflammation as detrimental, but emerging data in humans and mice reveal that ILC2-centered interactions among the epithelium, nervous system, and immune cells can modulate inflammation to repair tissue and restore homeostasis.
Ziyi Yin and Yawen Zhou, the first class of clinical medicine undergraduates at the SUSTech School of Medicine, have recently published a review article on the cutting-edge advances in epithelial-immune and neuro-immune interactions. In particular, it looks at how ILC2s modulate the pathogenic process of barrier diseases. This work was supervised by Quan Liu, Associate Professor of Biochemistry at the SUSTech School of Medicine.
Their article, entitled “Neuro-epithelial-ILC2 crosstalk in barrier tissues,” has been published in Trends in Immunology, a renowned review journal in immunology with a 5-year impact factor of 21.1. This review piece is the only featured article of the current issue.
Barrier tissues (including skin, respiratory tract, and gastrointestinal tract) are the first defense against internal and external changes. Damaged barrier tissues trigger inflammation to remove pathogens and promote tissue repair, and ILC2 plays a unique and central role in this process: integrating epithelial signals (e.g., IL-33, IL-25, TSLP, etc.) and neural signals (neurotransmitters and neuropeptides) to modulate the tissue microenvironment and the inflammatory process.
Atopic dermatitis, asthma, acute respiratory distress syndrome, and inflammatory bowel disease are major medical burdens globally. This review focuses on the three major barrier tissues mentioned above. It discusses the regional neuroanatomical basis (especially the fibers that can receive external signal stimuli and release relevant neural signals, including TRPV1+ sensory fibers), the pathogenesis of these diseases, and especially the key role played by neuro-epithelial-ILC2 units.
This paper provides new ideas for basic biomedical research based on a neuro-epithelial-immune interaction network, and points out important scientific issues related to the clinical treatment and drug development of major diseases.
Ziyi Yin is the first author of this paper, and Dr. Quan Liu is the corresponding author.
This paper was supported by the National Natural Science Foundation of China (NSFC); Science, Technology and Innovation Commission of Shenzhen Municipality; Special Funds for the Cultivation of Guangdong College Students’ Scientific and Technological Innovation; and SUSTech College Students’ Innovation and Entrepreneurship Training Program.
Paper Link: https://doi.org/10.1016/j.it.2022.09.006
To read all stories about SUSTech science, subscribe to the monthly SUSTech Newsletter.
Proofread ByAdrian Cremin, Yingying XIA
Photo By