Hepatocellular carcinoma (HCC) accounts for more than 90% of primary liver cancer and remains a worldwide health problem due to its aggressive and lethal nature. Transarterial chemoembolization (TACE) is the first-line treatment for unresectable HCC. This treatment involves the embolization of tumor vessels and the delivery of high-concentration chemotherapy drugs, which are locally released into the tumor tissues to promote tumor necrosis. However, the therapeutic effect of this method has always been controversial. Therefore, designing an ideal embolization model to evaluate the pharmacokinetics inside the tumor site and accurately evaluate the therapeutic effects of clinically relevant embolization agents is of great significance.
Assistant Professor Qiongyu Guo’s team from the Department of Biomedical Engineering and Assistant Professor Xiaoying Tang’s team from the Department of Electronic and Electrical Engineering at the Southern University of Science and Technology (SUSTech) have recently collaborated on the publication of a visualized 3D tumor-mimicking chemoembolization model. The model, which combines deep learning and graph analysis methods, has made significant progress in the construction of an ex vivo organ-structured evaluation platform for liver cancer chemoembolization treatment.
Their research results, entitled “A 3D Tumor-Mimicking in Vitro Drug Release Model of Locoregional Chemoembolization Using Deep Learning Based Quantitative Analyses,” have been published in Advanced Science.
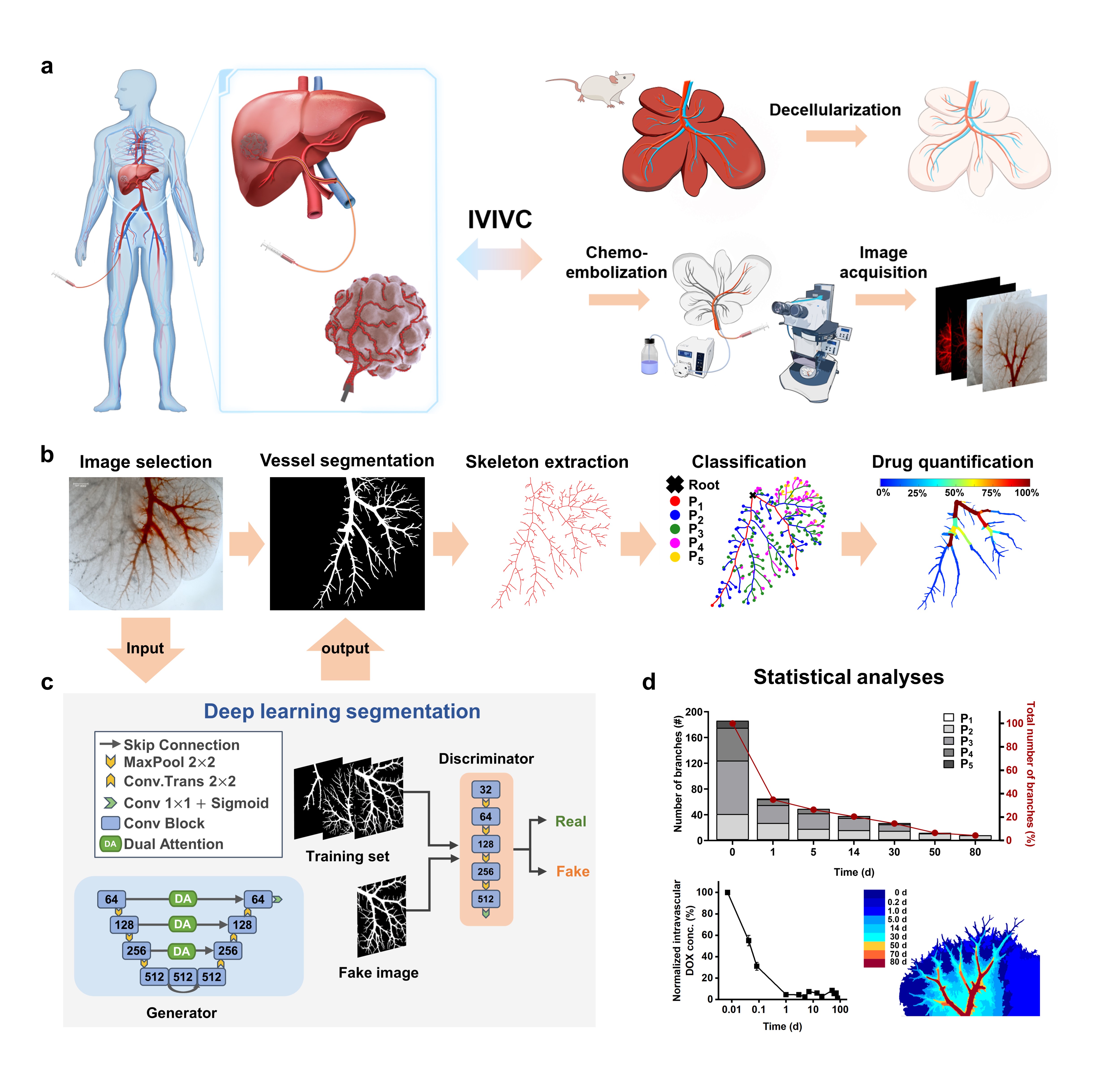
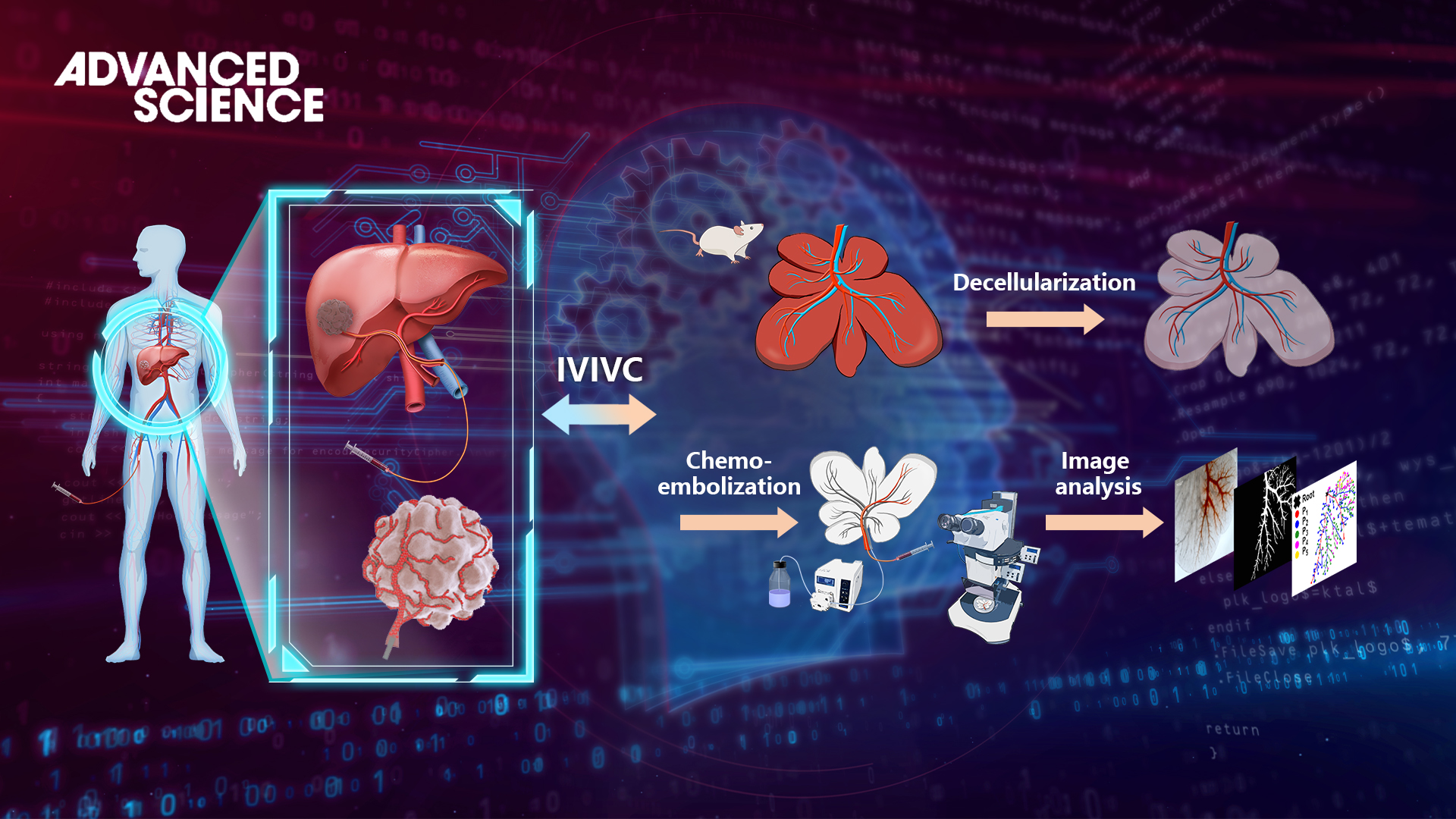
Figure 1. Schematic diagram of the 3D embolization model based on deep learning.
Prof. Qiongyu Guo’s and Prof. Xiaoying Tang’s teams collaborated to design a 3D tumor-mimicking drug release model through utilizing decellularized liver organ as a drug-testing platform (Figure 1). The model contains three key features that affect drug release in vivo: a complex vascular system, a drug-diffusible electronegative extracellular matrix, and controllable drug depletion. This drug release model, combined with deep learning-based computational analyses for the first time, permits quantitative evaluation of all important parameters associated with locoregional drug release. The U-shaped segmentation network based on attention mechanism and adversarial training can achieve accurate segmentation of the embolized vascular region with few annotated samples.
A series of image processing and graph analysis algorithms were combined to achieve an accurate and automatic quantitative statistical analysis of drug loss. To further verify the feasibility and accuracy of the model, the study quantitatively analyzed the endovascular embolization distribution, intravascular drug retention, and extravascular drug diffusion, establishing an in vivo-in vitro correlation with in-human results up to 80d.
Using the established 3D tumor-mimicking model, the in vitro chemoembolization efficacy of three different formulations of doxorubicin solution was systematically evaluated (Figure 2). The researchers used image processing algorithms to extract the skeleton of the segmented embolized vessels and constructed a custom multi-level tree. Subsequently, quantitative analysis and statistical comparison were performed at different tree levels, allowing for a clear depiction of the differences in embolization depth and changes in residual drugs within blood vessels for the three formulations over 80 days.
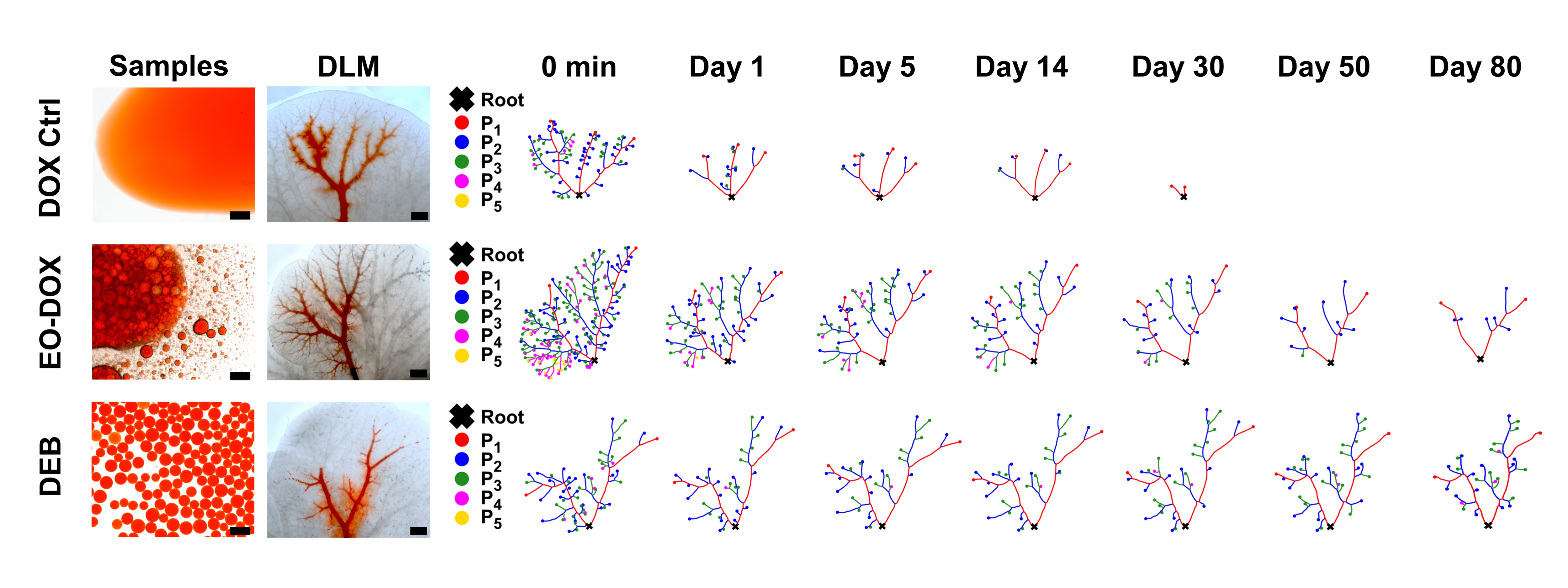
Figure 2 Vessel topological analyses. Skeleton extraction and classification of drug-containing vessels of three drug formulations, i.e., DOX Ctrl, EO-DOX, and DEB, tested in the DLM model over 80 d. DOX: doxorubicin solution; EO-DOX: an emulsion of ethiodized oil and doxorubicin solution; DEB: drug-eluting bead.
The local drug concentration within tumors is an important factor in determining their therapeutic efficacy. Taking advantage of the visualization capabilities of the 3D model and the strong self-fluorescence of doxorubicin at low concentrations, the researchers determined the extracellular drug diffusion depth as compared to the drug diffusion behavior observed in in vivo experiments. They found that the drug diffusion depth in this 3D model exhibited great linearity with the in-human results, validating the effectiveness of the embolic chemotherapy model for in vivo–in vitro consistency evaluation. This has important guiding significance for the development of new drug formulations and evaluation of embolic chemotherapy efficacy in clinical practice (Figure 3).
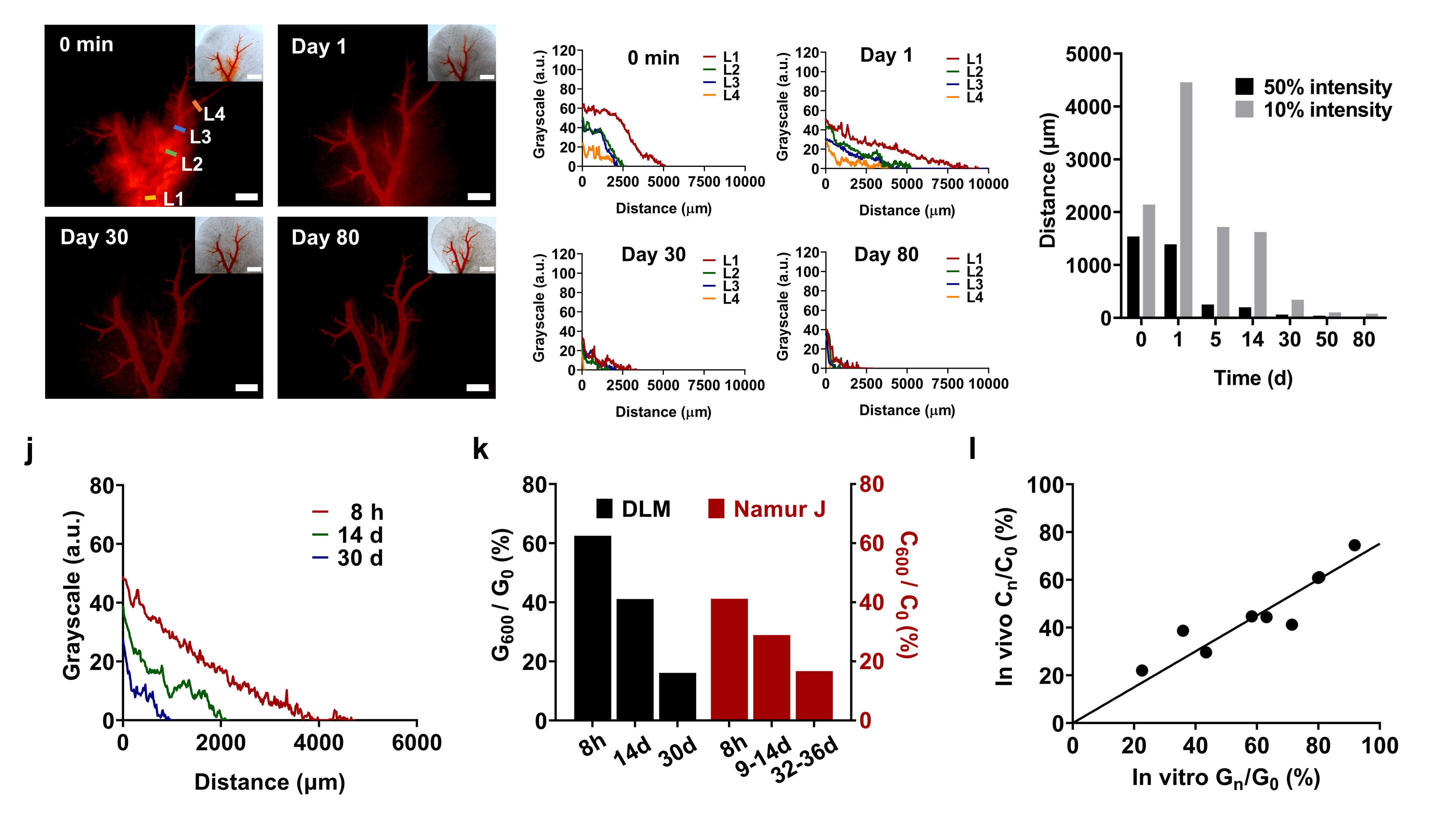
Figure 3 Extravascular drug diffusion of drug-eluting beads in DLM model and IVIVC.
Dr. Xiaoya Liu, a postdoctoral fellow from the Department of Biomedical Engineering at SUSTech, and Xueying Wang, a master’s student from the Department of Electronic and Electrical Engineering at SUSTech, are the first authors of this paper. Asst. Prof. Qiongyu Guo and Asst. Prof. Xiaoying Tang are the corresponding authors. SUSTech is the corresponding institution of the paper. Other collaborating authors included master’s students Yucheng Luo, Meijuan Wang, and Xiaoyu Han, all from SUSTech.
This work was supported by the National Natural Science Foundation of China (NSFC), Guangdong Innovative and Entrepreneurial Research Team Program, Science, Technology and Innovation Commission of Shenzhen Municipality, and SUSTech.
Paper link: https://onlinelibrary.wiley.com/doi/10.1002/advs.202206195?af=R
To read all stories about SUSTech science, subscribe to the monthly SUSTech Newsletter.
Proofread ByAdrian Cremin, Yingying XIA
Photo By